Psoriasis is a chronic autoimmune condition characterized by the rapid buildup of skin cells, leading to the formation of thick, red, and scaly patches on the skin’s surface. While it primarily affects the skin, psoriasis can also have significant implications for overall health and well-being. In this article, we will delve into how psoriasis affects your health, explore common symptoms, discuss treatment options, and examine the role of a podiatrist in managing this condition.
Understanding What is Psoriasis
Psoriasis affects approximately 2-3% of the global population, making it a relatively common condition. It occurs when the immune system mistakenly attacks healthy skin cells, triggering an accelerated growth cycle. As a result, new skin cells move to the surface of the skin too quickly, leading to the formation of thick patches known as plaques.
Impact on Health
Beyond its visible symptoms, psoriasis can have far-reaching effects on an individual’s physical and emotional well-being. Here are some ways in which psoriasis can impact health:
- Skin Discomfort: The most obvious impact of psoriasis is the discomfort caused by the inflamed, itchy, and sometimes painful patches of skin. These symptoms can significantly affect mobility and quality of life.
- Psychological Impact: Living with a visible skin condition like psoriasis can take a toll on mental health. Many individuals experience feelings of embarrassment, self-consciousness, and depression, leading to decreased self-esteem and social withdrawal.
- Increased Risk of Comorbidities: Psoriasis is associated with an increased risk of developing other health conditions, such as psoriatic arthritis, cardiovascular disease, diabetes, and depression. Managing psoriasis effectively is crucial in reducing the risk of these comorbidities.
Common Symptoms of Psoriasis
Psoriasis can manifest in various forms, and symptoms may vary from person to person. However, some common signs and symptoms include:
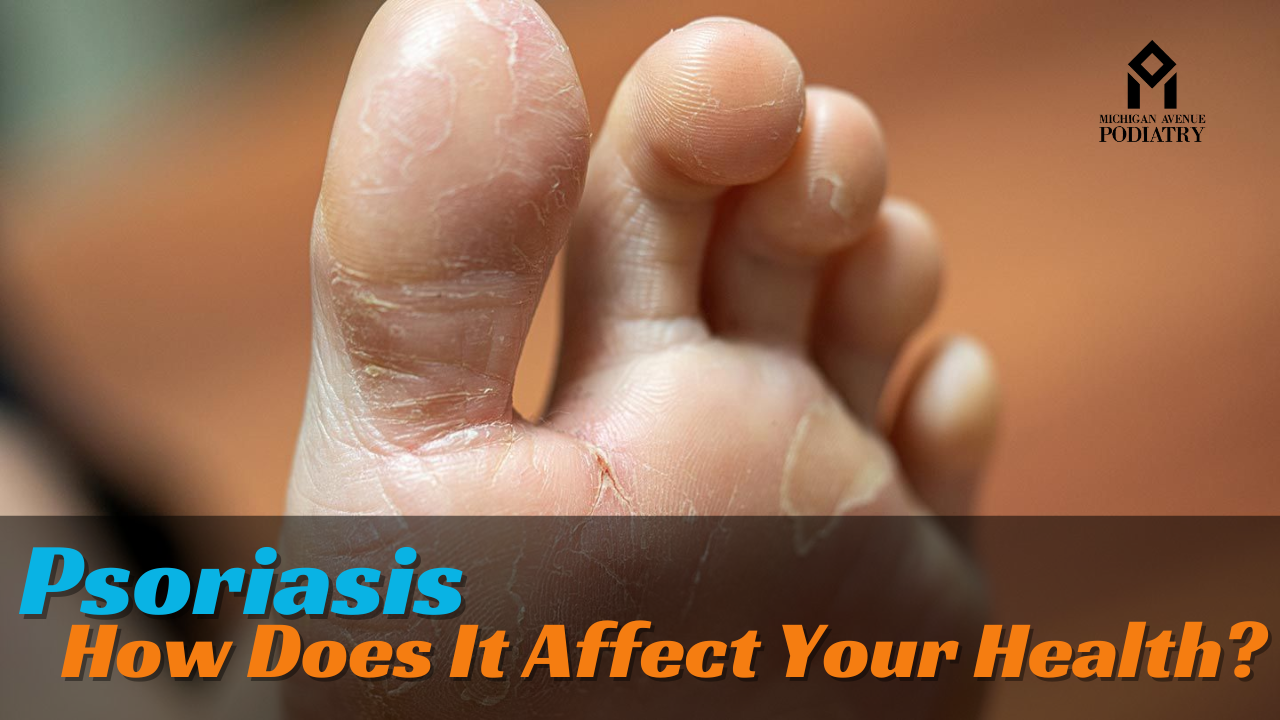
- Red, Scaly Patches: Raised, red patches of skin covered with thick, silvery scales are characteristic of psoriasis. These patches can appear anywhere on the body, including the scalp, elbows, knees, and lower back.
- Itching and Discomfort: Psoriasis plaques often itch or feel sore, leading to discomfort and irritation.
- Nail Changes: Psoriasis can affect the nails, causing them to become thickened, pitted, or ridged. In severe cases, nails may even detach from the nail bed.
- Joint Pain: In some individuals, psoriasis may also be accompanied by psoriatic arthritis, causing inflammation and pain in the joints.
Treatment Options
While psoriasis is a chronic condition with no known cure, various treatment options can help manage symptoms and improve quality of life. Treatment approaches may include:
- Topical Treatments: Creams, ointments, and lotions containing corticosteroids, vitamin D analogs, or retinoids can help reduce inflammation and slow down skin cell growth.
- Phototherapy: Exposure to ultraviolet (UV) light under medical supervision can effectively treat psoriasis by slowing down skin cell turnover and reducing inflammation.
- Systemic Medications: For moderate to severe psoriasis, oral or injectable medications may be prescribed to target the underlying immune response and reduce inflammation.
- Biologic Therapies: Biologic drugs, which are derived from living organisms, target specific components of the immune system involved in psoriasis.
Role of a Podiatrist
While psoriasis primarily affects the skin, it can also impact the nails and joints, particularly in the case of psoriatic arthritis. A podiatrist, or foot specialist, plays a crucial role in managing psoriasis-related foot problems, such as:
- Nail Care: Podiatrists can assess and treat psoriasis-related nail changes, including thickening, pitting, or separation from the nail bed.
- Joint Pain Management: Individuals with psoriatic arthritis may experience foot and ankle pain due to inflammation in the joints. Podiatrists can provide treatments to alleviate pain and improve mobility.
- Custom Orthotics: Podiatrists may recommend custom orthotic devices to provide support and reduce pressure on affected joints, enhancing comfort and mobility.
Conclusion
Psoriasis is more than just a skin condition—it can have profound effects on both physical and mental health. Understanding the impact of psoriasis on overall health is crucial for effective management and treatment. By recognizing symptoms, exploring treatment options, and seeking support from healthcare professionals, individuals living with psoriasis can better manage their condition and improve their quality of life.
Incorporating the expertise of healthcare providers like podiatrists can further enhance the management of psoriasis-related complications, ensuring comprehensive care for those affected by this chronic condition.